For Keck Medicine of USC patients who need a post-operative tracheostomy tube, a well-trained nurse could be their best line of defense.
“Nurses are often the first to confront any post-op complications that can arise,” said Mark Swanson, MD, a head and neck surgeon at Keck Medicine of USC and assistant professor of clinical otolaryngology – head and neck surgery at the Keck School of Medicine of USC. “We want all nurses who watch over our patients to become experts in trach care.”
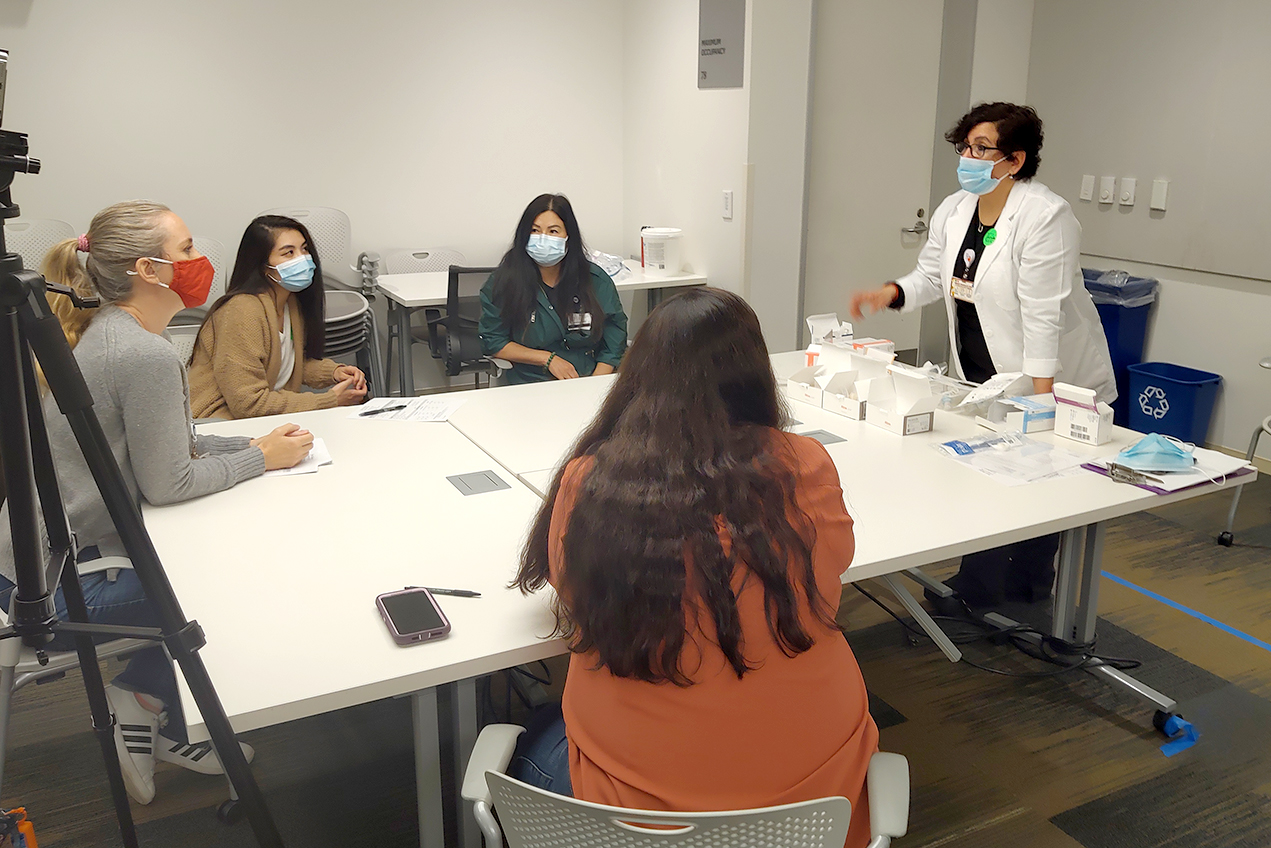
Together with Tamara Tervinskaya, BSN, RN, nursing professional development practitioner, Swanson recently created a trach training course for a group of Keck Medicine nurses dedicated to caring for patients seen by clinicians in the USC Caruso Department of Otolaryngology-Head and Neck Surgery, to give them a hands-on education in tracheostomy care.
“We want to empower our nurses so they feel confident and have the most up-to-date information,” Tervinskaya said.
The two-hour in-person course — a break from the solely virtual trainings once dictated by the pandemic — took place twice every Thursday throughout April. Before devising the curriculum, the Nursing Professional Development Department launched a monthly house-wide lecture series where the otolaryngology team lectured on such topics as laryngology, sleep apnea and trach care.
Assistant nurse manager Nicole Gilmore, BSN, RN, assisted with scheduling for the small-group workshops, each limited to about nine participants. After the video trach care lecture, nurses took part in three skill stations, starting with suctioning techniques to remove mucus and secretions, led by Daniel Motamedi, respiratory care practitioner/educator. At a trach equipment station, nurse navigator Daphne Bautista, MSN, RN, gave nurses a close-up look at the wide variety of trach tubes they may encounter. The final station — case studies, led by Swanson and physician assistant Christine Park — was designed to hone and encourage critical thinking.
For some of the nurses, working with tracheostomy equipment was a new experience. For others, the training served as a refresher and a chance to share what they know. Among the topics of discussion was the nurse’s role in educating patients in at-home trach care.
“Patients tend to do better at home,” Swanson said, “so it’s important they feel comfortable with the equipment and procedures.” He hopes to formalize the patient education component in future, part of a mission to prevent hospital readmissions.
Tervinskaya is tracking post-course improvements in care and plans to expand the training to other specialties. The trach training got high marks from its students.
“Ultimately the more informed nurses are,” Tervinskaya said, “the higher quality care they can provide our patients.”
— Candace Pearson