Keck School of Medicine of USC researchers have identified a human protein that could prevent cancer by restricting a type of herpes virus from replicating.
The scientists examined the human herpes virus 8, otherwise known as Kaposi sarcoma-associated herpesvirus. Kaposi sarcoma is a cancer that causes lesions in soft tissue, including skin, the oral cavity, lymph nodes and internal organs.
Shou-Jiang Gao, PhD, senior author of the study, has been studying this eighth type of herpes viruses for almost 25 years. The current study, published in Nature Microbiology on Nov. 6, is the first to map healthy cells and those infected by a large DNA virus, Gao said.
“Understanding how the herpes virus switches from being dormant to causing cancer is important because of the health problems the herpes virus causes worldwide,” said Gao, a professor of molecular microbiology and immunology at the Keck School.
More than 3.7 billion people under 50 years old — 67 percent of the population — are infected with two common herpes viruses that cause genital herpes or cold sores around the mouth, according to the World Health Organization.
Most herpes viruses remain dormant until someone’s immune system weakens due to factors such as age or a disease like human immunodeficiency virus or HIV. When the immune system cannot keep diseases in check, some of these herpes viruses can cause cancers.
“The findings from this study can potentially be translated into novel therapeutic approaches for cancers that are caused by viral infections,” Gao said.
Kaposi sarcoma is more common among people with HIV, transplant recipients and men of African descent. In some areas of Africa, more than 90 percent of the population shows signs of herpes virus 8 infection, according to the American Cancer Society.
Roadmap to cure viral-induced cancer
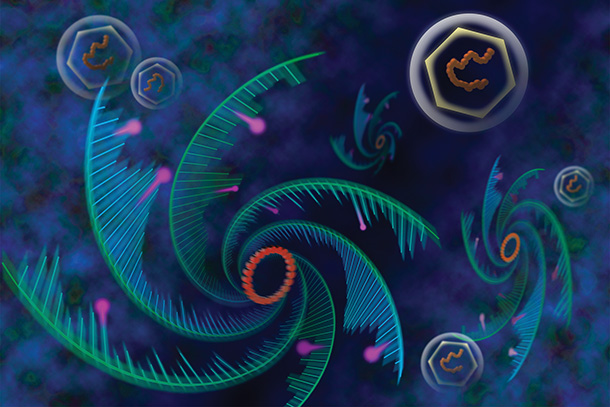
Scientists looked at messenger RNAs, which carry genetic messages from DNA to help make proteins — long chains of amino acids that form structural components of body tissue such as muscle and hair. Specifically, they studied N6-methyladenosine (m6A) and N6, 2-O-dimethyladenosine modifications to messenger RNAs.
Through mapping proteins that can restrict viral infections, the researchers found a protein called YTHDF2 that can help regulate the human herpes virus 8 by detecting the m6A modification on viral messenger RNA. The protein is the key switch that regulates human herpes virus 8 replication.
“How the virus infects and replicates has a direct influence on how the cell becomes a cancer cell,” Gao said, adding that you cannot cure cancer without some kind of roadmap. “If a person has a disease and the problem area is in the hand, you wouldn’t want to treat the head. That’s why you need to map the disease pathway. In this case, the YTHDF2 protein detects the m6A modifications on messenger RNAs.”
Brandon Tan from the Keck School of Medicine was the lead author of the study. Hui Liu, Suzane Ramos Silva, Hongfeng Yuan and Océane Sorel from the Keck School of Medicine; Songyao Zhang, Lin Zhang, Xiaodong Cui and Yufei Huang from the University of Texas at San Antonio; and Shaowu Zhang from Northwestern Polytechnic University also contributed to this study.
The study was completely supported by the federal government with National Institutes of Health grants totaling $300,000 (CA096512, CA124332, CA132637, CA213275, CA177377, DE025465, CA197153 and GM113245).
— Zen Vuong