A new interdisciplinary USC study shows that an antidepressant in use for decades, repurposed to fight prostate cancer, could help patients whose disease has returned following surgery or radiation.
The drug — an MAO inhibitor called phenelzine — represents a potential new treatment direction with fewer side effects for men with recurrent prostate cancer, researchers said.
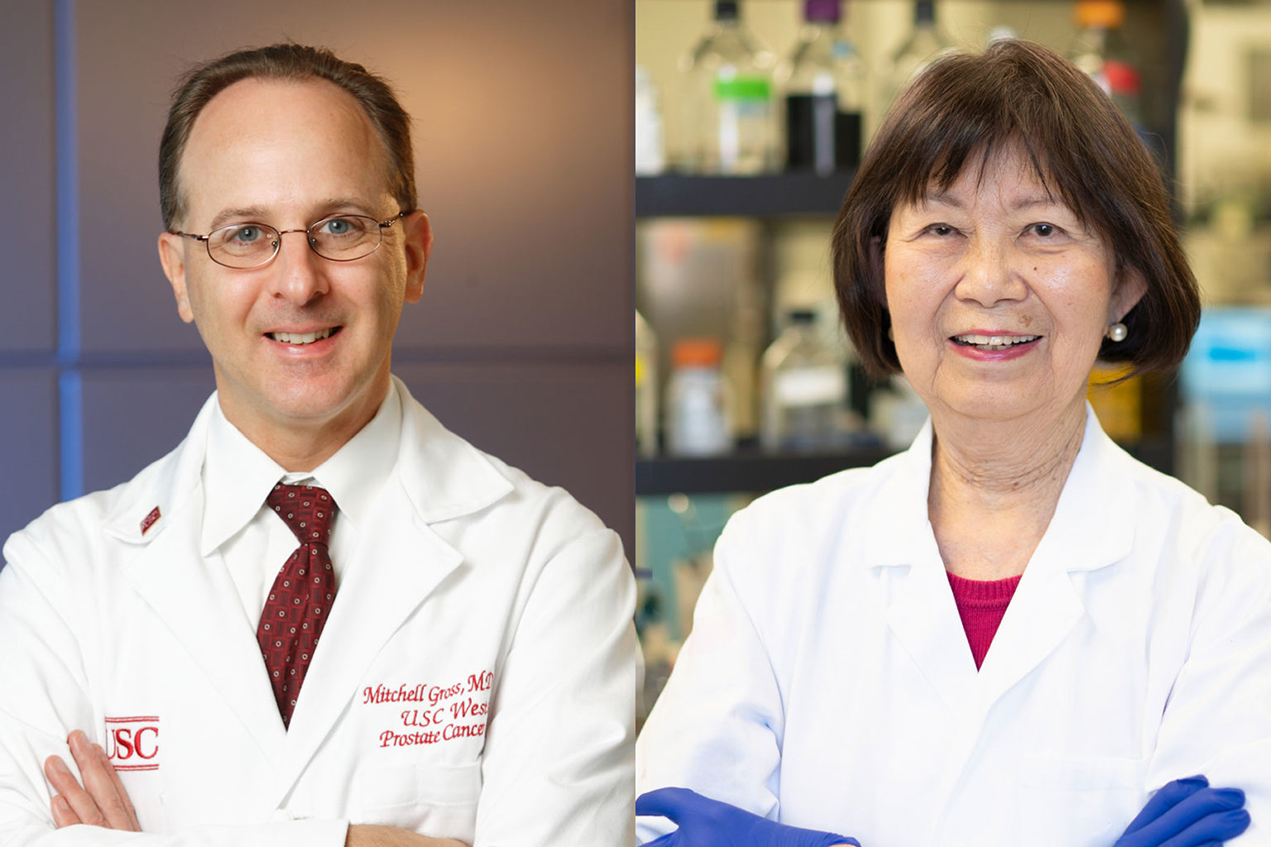
“To our knowledge, this study is the first clinical trial of an MAO inhibitor in cancer patients,” said senior author Jean Shih, PhD, a University Professor at the USC School of Pharmacy who has studied the enzyme MAO, or monoamine oxidase, for four decades.
The research appears in the journal Prostate Cancer and Prostatic Diseases.
“If our findings are confirmed, this could part of a new avenue for patients that could avoid undesirable side effects of standard therapies,” said first author Mitchell Gross, MD, PhD, a medical oncologist and research director at the Lawrence J. Ellison Institute for Transformative Medicine of USC. Gross and Shih have been collaborating for several years to bring her research out of the lab and into the clinic.
In this study, 11 of 20 participants had a measurable decline in their PSA levels after 12 weeks of twice-a-day treatment, with the greatest decline in PSA being a 74% drop. PSA stands for prostate-specific antigen; it’s a biomarker for prostate cancer circulating in the blood.
How MAO inhibitors can help prostate cancer patients
Prostate cancer is the second most common cancer — behind skin cancer — diagnosed in men in the United States, with about 174,000 cases diagnosed each year. For most patients, prostate cancer is treated with surgery, radiation or a combination of the two.
After surgery, a patient’s PSA should be close to zero. However, in about one-third of patients, the PSA level rises again, indicating the cancer has returned. Hormone therapy is a standard treatment for recurrent prostate cancer, but it comes with serious side effects that impact quality of life.
That’s where MAO inhibitors may be able to help.
MAO inhibitors treat depression by readjusting levels of neurotransmitters such as serotonin and dopamine in the brain. The downside is that the medication requires dietary changes and careful avoidance of drug interactions to prevent serious side effects.
In prostate cancer, MAO inhibitors disrupt androgen receptor signaling — the main growth pathway for prostate cancer. Previous studies with animals and human prostate cancer cell lines showed that MAO inhibitors decreased the growth and spread of prostate cancer, the researchers found.
Because the MAO inhibitor phenelzine is already FDA-approved, the researchers were able to rapidly design and implement a pilot study to test the drug’s ability to fight cancer.
Antidepressant lowers PSA levels
For this study, researchers enrolled 20 participants who had been treated for prostate cancer and who had elevated PSA levels. Patients received the MAO inhibitor phenelzine twice a day for 12 weeks. Fifty-five percent of the men experienced PSA declines; five of them saw PSA level declines of 30% or more; two participants saw decreases of 50% or more.
Three patients had to drop out due to dizziness or hypertension.
The main limitations of the study include the lack of a placebo comparison group and the small sample size, researchers said. Additional studies are planned, and Shih has patented a second-generation MAO inhibitor tagged with a substance that could help doctors see where the cancer has spread.
In addition to Shih and Gross, other study authors are David Agus, MD, Olga Castellanos, CCRP, and Patrick Gilmore, MS, of the Ellison Institute; Tanya Dorff, MD, Jacek Pinski, MD, PhD, and David Quinn, MD, of the USC Norris Comprehensive Cancer Center at Keck Medicine of USC.
Shih holds the Boyd P. and Elsie D. Welin Professorship in Pharmacology and Pharmaceutical Sciences at the USC School of Pharmacy and is director of the USC-Taiwan Center for Translational Research at the USC School of Pharmacy. She is a two-time winner of the MERIT award from the National Institutes of Health.
In addition to his appointment at the Ellison Institute, Gross is an associate professor of clinical medicine at the Keck School of Medicine of USC and research director of the USC Norris Westside Cancer Center.
— Leigh Hopper
The study was supported with funding from the USC-Taiwan Center for Translational Research, supported by the Tsai Family Fund, and National Cancer Institute grant P30CA014089.