The USC Institute of Urology, recently ranked in the top 15 Best Hospitals nationwide for urology by U.S. News and World Report, has received two grants from the National Institutes of Health to advance the field of prostate cancer diagnostics.
A $2 million research grant will examine the effectiveness of using magnetic resonance (MR)-ultrasound image fusion technology to diagnose clinically significant prostate cancer in African-American versus Caucasian men. This is the first prospective, randomized comparison of standard biopsies versus targeted biopsies in these two ethnic groups.
MR-ultrasound image fusion combines magnetic resonance and ultrasound imaging to identify potentially aggressive lesions prior to biopsy. Physicians could then select two or three targets for a needle biopsy, or perhaps rule out the need for a biopsy altogether.
The method is being incorporated slowly in prostate cancer diagnostics, primarily at centers of excellence like the USC Institute of Urology. However, the current widespread practice involves 12-14 random needle biopsies, which may cause patients negative side effects. Moreover, the randomness of this procedure may lead to inaccurate results — cancerous lesions are not localized uniformly within each prostate and more aggressive lesions might not be biopsied.
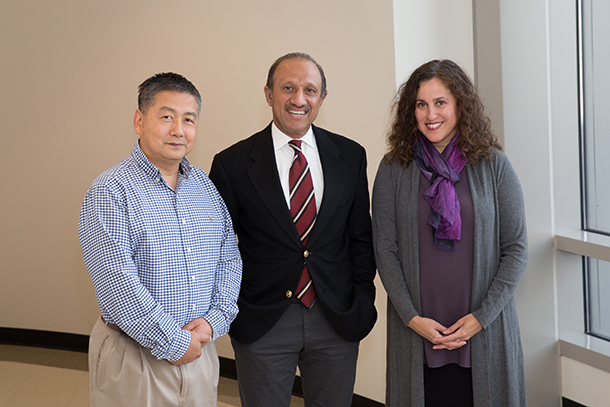
“Because of the side effects associated with diagnosing and treating prostate cancer, there is a fine line between vigilance and overtreatment,” said Inderbir Gill, MD, MCh, founding executive director of the USC Institute of Urology, chair and professor of urology at the Keck School of Medicine of USC and a principal investigator of the study. “If this method proves successful, physicians can walk that line more precisely, decreasing patient risk while improving accuracy.”
The research effort focuses specifically on African-American men because of their increased risk for the disease. According to the American Cancer Society, prostate cancer occurs more often in African-American men than in other ethnicities. Prostate cancer is also more aggressive among African-Americans, who are twice as likely to die of the disease than Caucasian men.
“Too many men are getting biopsies, and few are choosing active surveillance, in particular African-American men because they are more at risk for prostate cancer and having clinically significant disease missed at the time of biopsy,” said Mariana Stern, PhD, associate professor of research preventive medicine and urology and a co-principal investigator of the study. “Developing a targeted method for diagnosis would give men more confidence in making treatment decisions and potentially decrease the number of prostate biopsies.”
A second exploratory grant will assess whether or not DNA methylation in prostate cancer biopsy tissue can accurately determine if a prostate cancer lesion is aggressive. DNA methylation creates detectable marks that are altered when tumors develop. Aggressive cancer cells typically cause more alterations. If successful, this practice could provide clinicians and patients additional insight as to the best course of prostate cancer treatment.
“Although prostate cancer treatment can sometimes negatively impact patients’ quality of life, many patients have non-aggressive cancers that do not require initial treatment,” said Gangning Liang, MD, PhD, professor of research urology at the Keck School. Liang is a principal investigator of this study alongside Gill. “This initiative takes research from the bench to the bedside, using correlations in basic science to provide patients the best standard of care.”
The USC Institute of Urology will begin recruitment for the studies this fall. They aim to recruit 400 participants in collaboration with five other prestigious research centers: Memorial Sloan Kettering Institute of Cancer Research; University of Maryland, Baltimore; Johns Hopkins University; Henry Ford Health System; and University of Texas Southwestern Medical Center.
— Mary Dacuma