USC research sheds new light on how a breakdown in the brain’s vascular system predates the accumulation of toxic plaques and tangles in the brain that bring about Alzheimer’s disease. The research suggests an earlier target for preventing dementia and Alzheimer’s.
Nearly 50 percent of all dementias, including Alzheimer’s, begins with the breakdown of the smallest blood vessels in the brain and their protective “gatekeeper cells,” according to a Keck School of Medicine of USC study.
That catastrophe causes a communications failure called small vessel disease. Many people with that disease also have white matter disease, the wearing away of fatty myelin that allows neurons to transfer messages within the brain network. In an animal model, researchers found that brain deterioration associated with dementia may start as early 40 in humans.
For more than 25 years, scientists have known that white matter disease impedes a person’s ability to learn or remember new things, slows thinking and causes people to fall more often due to balance issues. They identified a link between crippled small blood vessels in the brain and white matter disease but didn’t know what started that process until now.
“Many scientists have focused their Alzheimer’s disease research on the buildup of toxic amyloid and tau proteins in the brain, but this study and others from my lab show that the problem starts earlier — with leaky blood vessels in the brain,” said Berislav Zlokovic, MD, PhD, chair and professor of physiology and neuroscience, Mary Hayley and Selim Zilkha Chair in Alzheimer’s Disease Research, director of the Zilkha Neurogenetic Institute and senior author of the study.
“The collapse of pericytes — gatekeeper cells that surround the brain’s smallest blood vessels — reduces myelin and white matter structure in the brain. Vascular dysfunctions, including blood flow reduction and blood-brain barrier breakdown, kick off white matter disease.”
The role played by pericytes
The study, published in Nature Medicine on Feb. 5, explains that pericytes play a critical role in white matter health and disease via fibrinogen, a protein that circulates in blood. Fibrinogen develops blood clots so wounds can heal. When gatekeeper cells are compromised, an unhealthy amount of fibrinogen slinks into the brain and causes white matter and brain structures, including axons (nerve fibers) and oligodendrocytes (cells that produces myelin), to die.
Axel Montagne, PhD, first author of the study, said he and his colleagues are the first to show that fibrinogen is a key player in non-immune white matter degeneration. The protein enters the brain through a leaky blood-brain barrier.
“We demonstrated that controlling fibrinogen levels can, in a mouse model, reverse or slow white matter disease, the harbinger to dementia,” said Montagne, assistant professor of research physiology and neuroscience at the Keck School.
Dementia affects 50 million people worldwide and costs the world an estimated $818 billion, according to the World Health Organization.
As a research institution devoted to promoting health across the life span, USC has more than 70 researchers dedicated to the prevention, treatment and potential cure of Alzheimer’s disease and other dementias.
A new villain to target
The study found about 50 percent fewer gatekeeper cells and three times more fibrinogen proteins in watershed white matter areas in postmortem Alzheimer’s brains of humans compared to healthy brains.
To understand what was happening, USC-led researchers studied mice lacking in pericytes and compared them with a control group.
Using a MRI technique the Zlokovic Lab developed, they noticed 50 percent increased vessel leakage in mice that were 36 to 48 weeks old, roughly the equivalent of 70-year-old humans. The animal model replicated what scientists observed in the postmortem brains of people.
So they took a closer look.
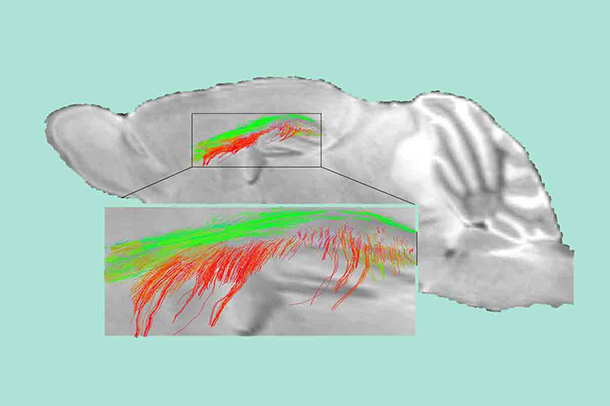
The scientists also found reduced cerebral blood flow and increased accumulation of fibrinogen in the brains of mice deficient in gatekeeper cells. At 12 to 16 weeks old, the experimental mice had 10 times more fibrinogen in the corpus callosum compared to the control group. That region is the brain’s central transit terminal that routes motor, sensory and cognitive information to their final destinations.
“Our observations suggest that once pericytes are damaged, blood flow in the brain reduces like a drain that is slowly getting clogged,” said Angeliki Maria Nikolakopoulou, PhD, co-first author of the study and assistant professor of research physiology and neuroscience.
On the wheel
Researchers had the mice run on a wheel to test their subcortical brain region, the same area studied in postmortem humans. At first, the wheel had equally spaced rungs. After two weeks, scientists removed some of the rungs. When the experimental group was 12 to 16 weeks old, they reached a maximum speed that was about 50 percent slower than the control group.
“The mice deficient in pericytes function slower because there are structural changes in their white matter and a loss of connectivity among neurons,” Zlokovic said.
The researchers used diffusion MRI techniques the Zlokovic Lab developed to see what was happening in the brain. They saw white matter changes in mice as early as 12 to 16 weeks old. Theoretically, that means white matter disease in humans could begin when they are just 40 years old, Montagne said.
“Pericytes are compromised early on,” Montagne said. “Think of it as hair clogging a drain over time. Once the drain is clogged, cracks begin forming in the ‘pipes’ or brain’s blood vessels. White matter frays and brain connections are disrupted. That’s the beginnings of dementia.”
Testing the poison
To confirm that fibrinogen proteins are toxic to the brain, researchers used an enzyme known to reduce fibrinogen in the blood and brain of mice. White matter volume in mice returned to 90 percent of their normal state, and white matter connections were back to 80 percent productivity, the study found.
“Our study provides proof that targeting fibrinogen and limiting these protein deposits in the brain can reverse or slow white matter disease,” Zlokovic said. “It provides a target for treatment, but more research is needed. We must figure out the right approach.
“Perhaps focusing on strengthening the blood-brain barrier integrity may be an answer because you can’t eliminate fibrinogen from blood in humans. This protein is necessary in the blood. It just happens to be toxic to the brain.”
Angeliki Nikolakopoulou, Zhen Zhao, Abhay Sagare, Gabriel Si, Divna Lazic, Anita Ramanathan, Ariel Go, Erica Lawson, Yaoming Wang, Jobin Varkey, Ralf Langen and Russell Jacobs from the Zilkha Neurogenetic Institute, Samuel Barnes from the California Institute of Technology, Madelaine Daianu and Paul Thompson from the Imaging Genetics Center at the USC Mark and Mary Stevens Neuroimaging and Informatics Institute, William Mack from the Keck School of Medicine, Julie Schneider from Rush University Medical Center and Eric Mullins from the University of Cincinnati College of Medicine also contributed to this study.
The federal government funded this research with about $6 million in grants from the National Institutes of Health (NS100459, AG039452, NS034467, AG023084). The remainder was funded by the Foundation Leducq Transatlantic Networks of Excellence (no. 16 CVD 05 and ES024936).