Fifteen percent of the U.S. population has chronic kidney disease. At its most severe, end-stage kidney disease (ESKD) requires patients to receive dialysis regularly or have a kidney transplant. According to the CDC, over 750,000 people in the U.S. are living with ESKD with over 70% receiving dialysis treatment regularly.
Most patients with ESKD receive health insurance through Medicare, which provides coverage for patients with kidney failure regardless of age. However, a growing segment of this population receives coverage through a private payer. Some policymakers have raised concerns that dialysis facilities are actively encouraging this trend by subsidizing ESKD patients’ individual market premiums in hopes of being paid more for their services.
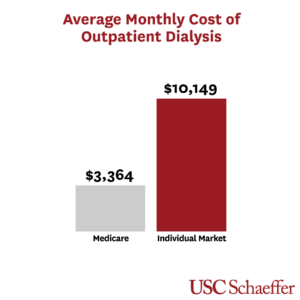
A new study published in JAMA Internal Medicine provides new information about dialysis spending in the individual market, finding that monthly spending on outpatient dialysis services for ESKD patients was three times higher for patients insured in the individual market compared to patients insured through Medicare.
“While most patients receiving dialysis are covered by Medicare, there are some concerns about whether dialysis facilities are instead steering patients to the individual market,” explained Erin Trish, PhD, associate director of the USC Schaeffer Center. “Our study shows that, even though the number of dialysis patients in the individual market is relatively small, because their spending is so high, this enrollment can actually raise premiums across the entire individual market.”
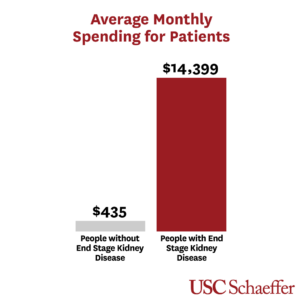
Patients with ESKD have average monthly spending 33 times higher than patients without
Trish and her colleagues leveraged a claims database comprising 28% of the 2016 ACA-compliant individual market. They find that patients with ESKD accounted for 0.1% of individual market enrollment but 3.3% of overall spending.
The average monthly spending on all health care services by patients with ESKD was $14,399 per individual — 33 times the spending by enrollees without ESKD.
The researchers find that individual market plans spent $10,149 per month on outpatient dialysis alone — over 300% of what Medicare pays.
“Such a large pay differential financially rewards dialysis facilities with more patients covered by the individual market,” added Eugene Lin, MD, MS, clinical fellow at the USC Schaeffer Center and assistant professor of medicine at the Keck School of Medicine of USC. “Facilities that encourage steering through subsidizing premiums would likely see a large increase in profits.”
There is reason for policymakers to act
Steering Medicare beneficiaries into the individual market would likely raise individual market premiums and increase the federal cost of subsidizing individual market coverage more than it reduced costs to the Medicare program, write the authors. Trish and her colleagues estimate that shifting 10% of non-elderly Medicare enrollees with end-stage kidney disease into the individual market would increase overall average individual market claims spending by over 4%.
But there are actions policymakers could take.
“The Centers for Medicare and Medicaid Services could revive an earlier effort to limit dialysis facilities’ steering efforts, or Congress could enact similar restrictions,” said Matt Fiedler, PhD, fellow at the USC-Brookings Schaeffer Initiative for Health Policy.
Ning Ning of the USC School of Pharmacy, Laura Gascue, MA, of the USC Schaeffer Center for Health Policy & Economics and Loren Adler of the USC-Brookings Schaeffer Initiative for Health Policy also authored the study. This study was supported by the USC-Brookings Schaeffer Initiative for Health Policy and the National Institutes for Health through the National Institute of Diabetes and Digestive and Kidney Disease (NIDDK).
— Stephanie Hedt


