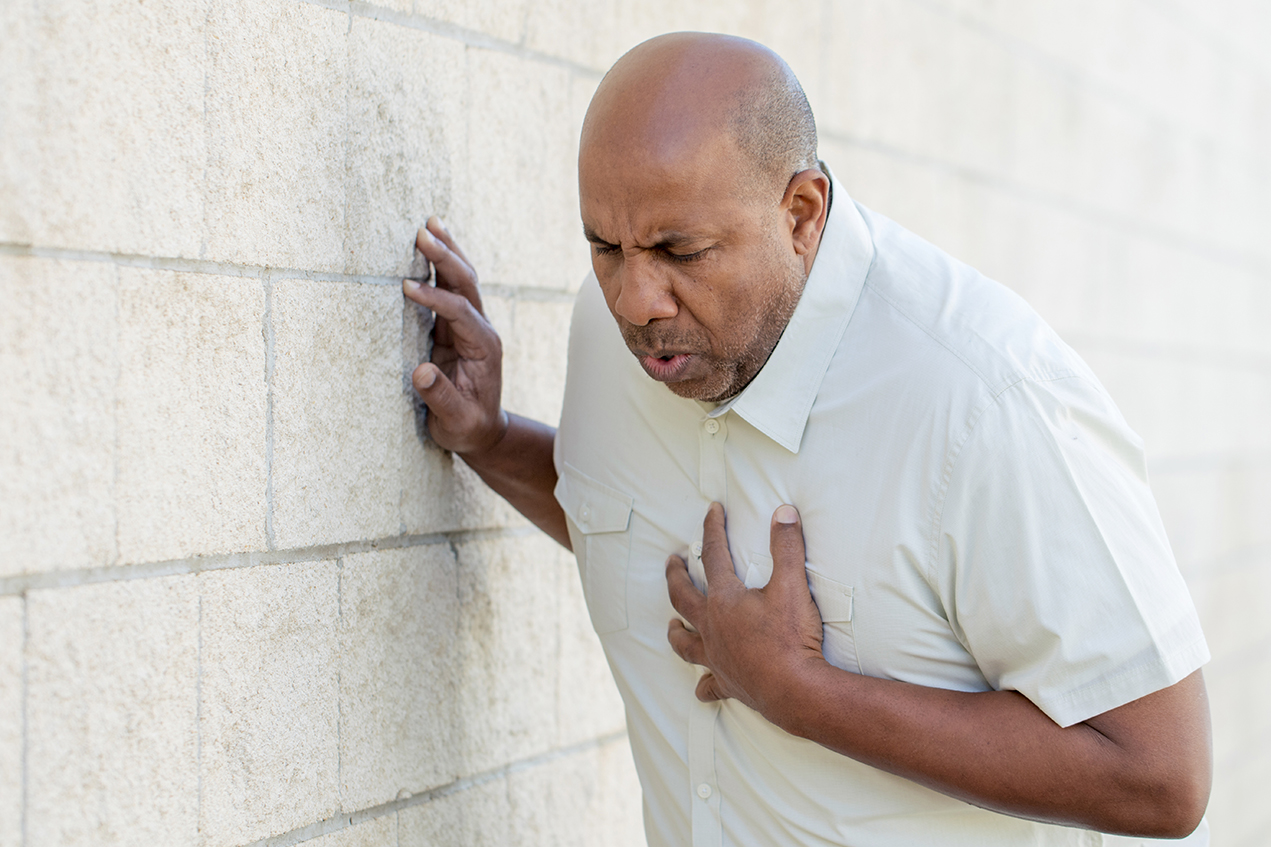
Every 40 seconds, someone in the United States has a heart attack — 805,000 Americans annually. For 75% of those individuals, it’s their first heart attack, making it difficult to act quickly in response to symptoms. At the same time, silent heart attacks (SMIs) account for 45% of heart attacks, meaning a large number of heart attack patients will mistake heart attack for a case of indigestion or even the flu.
Improving heart attack diagnosis and detection, especially in the case of an SMI, is crucial to reducing long-term health risks, health care expenses and morbidity rates. Niema Pahlevan, PhD, MS, assistant professor in the USC Viterbi Department of Aerospace and Mechanical Engineering, is creating a new approach that will allow patients to get treated earlier and hospitals to diagnose symptoms sooner as well.
Using fluid mechanics and applied mathematics, Pahlevan, who also holds a joint faculty appointment in the division of cardiovascular medicine at the Keck School of Medicine of USC, said you can detect biomarkers related to changing hemodynamics — fluid dynamics inside the veins, heart and arteries that help measure how well the heart is working. “We’re developing a monitoring system that uses these markers, but in a non-invasive and very uncostly way,” he said.
“We can use an iPhone or similar platform to perform monitoring and envision a device that would work like an at-home blood sugar test,” he said. In fact, Pahlevan has already developed a smartphone-based heart monitoring device. Now he’s working to accelerate the science behind it to make the device easier to accurately implement.
The device works by measuring vibrations produced by shifts in hemodynamics from the outside — for instance, the surface of your neck, along the carotid artery.
“A good portion of heart failure patients are not quickly diagnosed. On top of that, if they come to the hospital or clinic, they are often discharged too early, resulting in an early rehospitalization,” Pahlevan said. A diagnosis and monitoring tool that helps determine if individuals are experiencing a heart event — or if they’re on the brink of one — could save lives. In preventing repeat hospitalizations, it can also help save hospitals, Medicare and individuals time and money, he said.
“Approximately, eight billion dollars is wasted every year for unnecessary hospitalization of heart patients. So we’re tackling the health and economic pieces of the care for this type of patient in one device,” Pahlevan said.
Pahlevan was awarded a three-year American Heart Association (AHA) Career Development Award in support of this work. Pahlevan will conduct the clinical portion of the study in the Cardiac Catheterization Laboratory of Ray Matthews, MD, professor of clinical medicine at the Keck School.
How do you diagnose a heart attack?
A “classic” heart attack shows up with symptoms such as arm and chest pain, nausea and shortness of breath. However, not all symptoms are created equal, particularly in the case of SMIs. When a silent myocardial infarction occurs, sometimes even an EKG will fail to detect it.
To this end, Pahlevan and his team are developing biomarkers that enable them to measure the hemodynamic index referred to as the Left Ventricular and Diastolic Pressure (LVEDP) — a key indicator of heart health.
“When LVEDP goes up, we know it’s time to intervene. But since LVEDP reflects the pressure inside the heart at the end of the diastolic phase — in other words, the pressure inside the closed chamber — the only way to measure it is to put a catheter in through the groin (femoral artery) or wrist (radial artery), which is a highly invasive procedure,” Pahlevan said.
“Instead, we’ve tried to measure this pressure non-invasively using inexpensive devices, say under $100, that can work with existing platforms, like an iPhone.” By contrast, an MRI, which uses powerful magnets and radio waves to make pictures of your heart as it’s beating, can cost $2,500 on average for each heart scan.
The aorta is the major artery coming of the heart. The pressure and flow waves going into other vasculature create wave reflections, Pahlevan said. “These waves carry energy and information. What we’re doing is trying to understand this wave dynamics and develop mathematical tools to extract information from these waves.”
When waves propagate inside vessels, the vessel walls distend, imposing vibrations toward the skin’s surface. The device and the iPhone App that Pahlevan and his collaborators have designed will measure this vibration and from it, make a reading of the pressure inside the heart.
Time to Balloon
One of the main and most important issues in the survival rate of heart attack patients is what is referred to as the “time to balloon,” Pahlevan said. This measures how long it takes for a patient to get their heart vessels (coronary arteries) opened once they arrive at the hospital. However, Pahlevan said, a major area of focus is now from “symptom to door.”
In the case of a “classic” case of heart failure where expected signs like chest and arm pain are present, patients still tend to wait too long to call 911 and seek treatment. Meanwhile, in the case of SMIs, symptoms can easily be misinterpreted — especially in younger patients.
According to the American Heart Association, for every single minute a person waits between the time they feel symptoms to the time they are treated, heart cells could be irreversibly dying. “The first hour after a patient feels symptoms is crucial in reviving the patient and producing a positive long-term outcome,” Pahlevan said.
Pahlevan said the device they are developing has shown early results demonstrating it measures ejection fraction of the heart — the percentage of blood leaving your heart each time it contracts — more accurately than an echocardiogram and a good lower-cost competitor to an MRI.
“This monitoring device can make health care more accessible and affordable for a wider population, while reducing the mortality rate of heart attack patients and improving their outcomes,” Pahlevan said.
— Avni Shah