USC scientists are part of a team working on a smartphone app and cloud services platform that will predict the probability of a child’s future asthma attack and provide personalized risk management advice.
Frank Gilliland, MD, MPH, PhD, professor of preventive medicine at the Keck School of Medicine of USC, said the integrative Biomedical Real-Time Health Evaluation (BREATHE) platform he and colleagues from UCLA are developing is a potentially revolutionary approach to managing asthma, one of the most common chronic childhood diseases.
“We think this is the future for asthma care,” said Gilliland, co-principal investigator of the project. “We will use real-time, high-volume information about physiology, symptoms, medication use and environmental exposures. This ‘big data’ will help physicians manage patients better and prevent exacerbations. It is a personalized medicine approach that evaluates potential real-time environmental triggers, genetics and a child’s asthma attack history.”
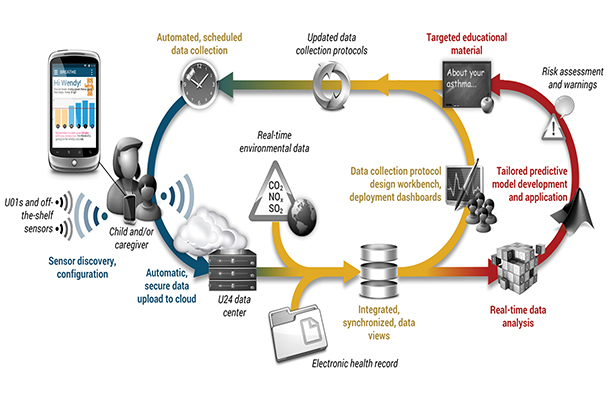
(Graphic/Alex Bui)
Researchers from both universities will build a platform that will crunch data from children’s wearable devices, smartphones and individual electronic health records as well as real-time reports on weather conditions, air quality, pollen and allergy forecasts, and other “asthma triggers.” The algorithm will supply contextual information in a secure, cloud-based system.
The National Institute of Biomedical Imaging and Bioengineering awarded a $5.25 million grant to co-principal investigators Gilliland and Jose-Luis Ambite, a research assistant professor in the Department of Computer Science at the USC Viterbi School of Engineering. The agency also awarded UCLA a $6 million grant, of which $1.85 million is expected to be subcontracted to USC. The money in both grants will be spread across four years of research and development.
About 6.8 million children in the United States have asthma, according to the Centers for Disease Control and Prevention. The currently incurable respiratory condition cost the United States about $56 billion in medical costs, lost school and work days in 2007.
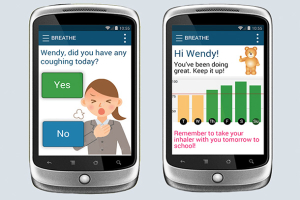
“Asthma weighs heavily on the nation in terms of public health, medical costs and quality of life,” said Alex Bui, PhD, also a principal investigator in this study and professor of radiological sciences at the David Geffen School of Medicine at UCLA. “One of the biggest challenges will be making the smart device user-friendly for young children. Kids like intuitive interfaces with bright colors, simple language, big text and quirky noises. We’re having fun exploring how to build those facets into our design.”
Researchers will test the platform on 8- to 12-year-old children with asthma. The algorithm scientists are developing will analyze data from the landmark USC Children’s Health Study, a litany of contextual data from environmental sensors and a history of previous asthma attacks. When exacerbating conditions arise again, the asthma app may remind a child or caregiver to bring an inhaler or medicine to ward off a future asthma attack.
“We will use technology to help people maximize their health and reduce the burden of childhood asthma,” said Gilliland, director of USC’s Division of Environmental Health. “Privacy is critical. The data has to be encrypted and secure so people could be assured their data will be confidential.”
— Zen Vuong