Paralyzed from the neck down after suffering a gunshot wound when he was 21, Erik Sorto now can move a robotic arm just by thinking about it.
Through a clinical collaboration among the California Institute of Technology, Keck Medicine of USC and Rancho Los Amigos National Rehabilitation Center, Sorto at 34 is the first person to have a neural prosthetic device implanted in a region of the brain where intentions are made, giving him the ability to perform a fluid hand-shaking gesture, drink a beverage and even play “rock, paper, scissors” using a robotic arm.
Neural prosthetic devices previously have been implanted in the brain’s movement center, the motor cortex, allowing patients with paralysis to control the movement of a robotic limb. The motion, however, is delayed and jerky. Now, by implanting neuroprosthetics in the posterior parietal cortex (PPC), a part of the brain that controls not the movement directly but rather the intent to move, Caltech researchers have developed a way to produce more natural and fluid motions.
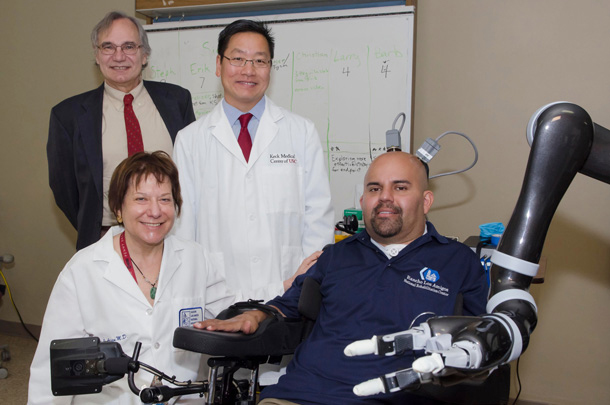
Designed to test the safety and effectiveness of this new approach, the clinical trial was led by principal investigator Richard Andersen, James G. Boswell Professor of Neuroscience at Caltech, neurosurgeon Charles Liu, professor of neurological surgery, neurology and biomedical engineering at USC and neurologist Mindy Aisen, chief medical officer at Rancho Los Amigos.
The device was surgically implanted in Sorto’s PPC at Keck Hospital of USC in 2013, and he since has been training with Caltech researchers and staff at Rancho Los Amigos to control a computer cursor and a robotic arm with his mind. The researchers saw just what they were hoping for: intuitive movement of the robotic arm.
Sorto, a single father of two who has been paralyzed for more than 10 years, was thrilled with the results.
“I was surprised at how easy it was [to control the robotic arm],” he said. “I remember just having this out-of-body experience, and I wanted to just run around and high-five everybody.”
Keck Medicine of USC surgeons performed the unprecedented neuroprosthetic implant in a five-hour surgery on April 17, 2013.
Liu and his team implanted a pair of small electrode arrays in two parts of the posterior parietal cortex — one that controls reach and another that controls grasp. Each 4-by-4 millimeter array contains 96 active electrodes that, in turn, record the activity of single neurons in the PPC. The arrays are connected by a cable to a system of computers that process the signals to decode the brain’s intent and control output devices, such as a computer cursor and a robotic arm.
“These arrays are very small so their placement has to be exceptionally precise, and it took a tremendous amount of planning — working with the Caltech team to make sure we got it right,” said Liu, who also is director of the USC Neurorestoration Center and associate chief medical officer at Rancho Los Amigos. “Because it was the first time anyone had implanted this part of the human brain, everything about the surgery was different: the location, the positioning and how you manage the hardware. Keep in mind that what we’re able to do — the ability to record the brain’s signals and decode them to eventually move the robotic arm — is critically dependent on the functionality of these arrays, which is determined largely at the time of surgery.”
The USC Neurorestoration Center’s primary aim is to turn scientific discoveries into effective therapies.
“We are at a point in human research where we are making huge strides in overcoming a lot of neurologic disease,” said Christianne Heck, associate professor of neurology at USC and co-director of the USC Neurorestoration Center. “These very important early clinical trials could provide hope for patients with all sorts of neurologic problems that involve paralysis such as stroke, brain injury, ALS and even multiple sclerosis.”
Sixteen days after his implant surgery, Sorto began training sessions at Rancho Los Amigos National Rehabilitation Center, where a computer was attached to the ports extending from his skull to communicate with his brain. Occupational therapists who specialize in helping patients adapt to loss of function in their upper limbs worked with Sorto and the Caltech team daily to help him visualize what it would be like to move his arm again.
Although he was able to immediately move the robot arm with his thoughts, after weeks of imagining, Sorto refined his control of the arm. Sorto now is able to execute advanced tasks with his mind, such as controlling a computer cursor.
Aisen, also a clinical professor of neurology at the Keck School of Medicine of USC, said that advancements in prosthetics like these hold promise for the future of patient rehabilitation.
“This research is relevant to the role of robotics and brain-machine interfaces as assistive devices, but also speaks to the ability of the brain to learn to function in new ways,” Aisen said. “We have created a unique environment that can seamlessly bring together rehabilitation, medicine and science as exemplified in this study.”
Sorto has signed on to continue working on the project for a third year. The study, he said, has inspired him to continue his education and pursue a master’s degree in social work.
“This study has been very meaningful to me,” Sorto said. “As much as the project needed me, I needed the project. It gives me great pleasure to be part of the solution for improving paralyzed patients’ lives. I joke around with the guys that I want to be able to drink my own beer — to be able to take a drink at my own pace, when I want to take a sip out of my beer and to not have to ask somebody to give it to me. I really miss that independence. I think that if it were safe enough, I would really enjoy grooming myself — shaving, brushing my own teeth. That would be fantastic.”
The results of the clinical trial appear in the May 22 edition of Science. The implanted device and signal processors used in the clinical trial were the NeuroPort Array and NeuroPort Bio-potential Signal Processors developed by Blackrock Microsystems in Utah.
The robotic arm used in the trial was the Modular Prosthetic Limb developed at the Applied Physics Laboratory at Johns Hopkins. Sorto was recruited to the trial by collaborators at Rancho Los Amigos National Rehabilitation Center and Keck Medicine of USC.
The trial was funded by the National Institutes of Health (grants EY013337, EY015545, P50MH942581A), the Boswell Foundation, the Department of Defense (contract N66001-10-4056) and the USC Neurorestoration Center.
Keck Medicine of USC team members include Brian Lee, Heck, Sandra Oviedo, Paul Kim and Meng Law. Caltech Andersen lab members include Tyson Aflalo, Spencer Kellis, Christian Klaes, Brian Lee, Ying Shi and Kelsie Pejsa. Rancho Los Amigos rehabilitation team members include Kathleen Shanfield, Stephanie Hayes-Jackson and Barbara Phillips.
Jessica Stoller-Conrad and Deborah Williams-Hedges of Caltech contributed to this story.
— Alison Trinidad