As the COVID-19 pandemic continues, Keck Medicine of USC employees and administrators are working extremely hard to respond to these rapidly changing circumstances. This ongoing series of stories will share the experiences of faculty and staff and their responses to the ongoing crisis.
This week, leadership and staff at USC Verdugo Hills Hospital discussed the preparations they’ve made, what patients can expect and what it’s like to be a clinician on the frontlines of the pandemic.

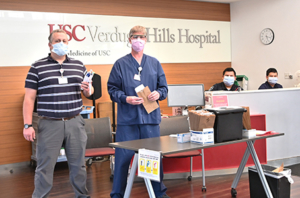
USC-VHH staff are working to preserve personal protective equipment as much as safely possible. (Photo/Catherine Pradt)
Planning and preparation
Months ago, USC-VHH leadership started discussing what to do if COVID-19 reached Southern California. The preparations that followed included a preemptive staffing level increase, supply procurement, technical advancements and staff orientations covering patient flow in the event of a surge.
“As an RN in the emergency department at USC-VHH, I can clearly see all of the time, treasure and talent leadership has put into preparation for this event,” said Richard Denogean, RN, BSN.
Transforming a hospital
Another important modification will make an immediate impression on patients: the transformation of the emergency department and its triage system. While many hospitals are building tents outside to manage an influx of potential COVID-19 patients, USC-VHH doesn’t have the outdoor space. Instead, the hospital is offering two separate emergency teams: a triage and care unit for people showing COVID-19 symptoms, and another for those experiencing more traditional emergencies.
David A. Tashman, MD, Emergency Room Department medical director and hospitalist for ED Services, explained that they are open for all patients in need. “We’re obviously still a fully functional emergency department, and we get all the normal stuff: cuts, sprains, falls, heart attacks, strokes,” he said.
The two types of patients will have separate entrances, both requiring screenings that will check for fever, other COVID-19 symptoms and a confirmed risk of exposure. Every patient will get a mask.
Traditional emergency patients will proceed to a designated area. Possible COVID-19 patients will go to the emergency department waiting room, which has been converted to a triage unit equipped with six patient pods designed for safety.
“We have six feet between patients,” explained Oscar Laurance-Munguia, RN. “We clean the area between patients and make sure that it’s well sanitized.”
The pods also are equipped with telemedicine tablets.
“If every patient had an in-person examination, not only the nurse but the doctor and everybody else would have to go through a glove, a gown, a mask, a bootie,” Tashman explained. “This way it minimizes the PPE, which, as I’m sure you heard, we’re trying to conserve as much as possible.”
Telemedicine also allows more physicians to be pulled in to help at a moment’s notice.
“Theoretically I could be anywhere,” Tashman said. “I could be doing this from home, if we had a surge of patients and needed extra doctors.”
Putting the patient at ease
The telemedicine system also allows for a faster assessment, which cuts down on wait times. Plus, the physicians have worked out how to accurately assess a patient’s condition via the tablets.
“We do have a full set of vital signs,” Tashman explained, “And just talking to you and asking you to do a few simple exercises like taking a deep breath in and out or counting to 10, I can get a good sense of whether you’re in any respiratory distress.”

Staff members stress that connection with the patient is a crucial part of recovery, regardless of the patient’s COVID-19 status. (Photo/Catherine Pradt)
For patients requiring further COVID-19 care, the staff is ready to provide the same level of compassion they would offer to any patient. Alyssa Levy, MS, speech pathologist, helps recently extubated patients to rehabilitate their swallow function, checks their vocal cord function and coughing abilities and monitors their functional breath work. She described connecting with patients as a crucial part of the recovery process.
“Even if I am covered in a gown, gloves, mask, hair bonnet and goggles, I am looking to connect with the person I am with, hold their hand, look into their eyes,” she explained. “With a good connection, everything else follows and this is the same as it ever was.”
Finding courage in uncertain times
In such trying times, the leadership and staff find that self-care and gratitude can be enormously helpful. Levy finds humor helpful, but also centers herself with meditation practice.
“Meditation has the ability to create peace and clarity for me and I rely on that spiritual connection especially when life is changing quickly and demands action,” she said. “Having a feeling of ‘deep roots’ gets me through.”
All arriving patients are screened carefully to make sure they’re not at risk for COVID-19 or the likelihood of infecting others. (Photo/Catherine Pradt)
For Denogean, comfort comes from “the love and support of my family, the community of excellent colleagues I am privileged to work with, and most of all my religious faith.”
Theresa Murphy, RN, MSHA, CENP, chief nursing officer at USC-VHH, expressed gratitude for those willing and able to help.
“We have received a lot of support from the community, and our Supply Management team is working tirelessly to source necessary materials. They have been heroes in the background for sure.”
People interested in donating supplies and materials to aid health care workers can visit KeckMedicine.org/coronavirus-donate for more information.
— Kate Faye


