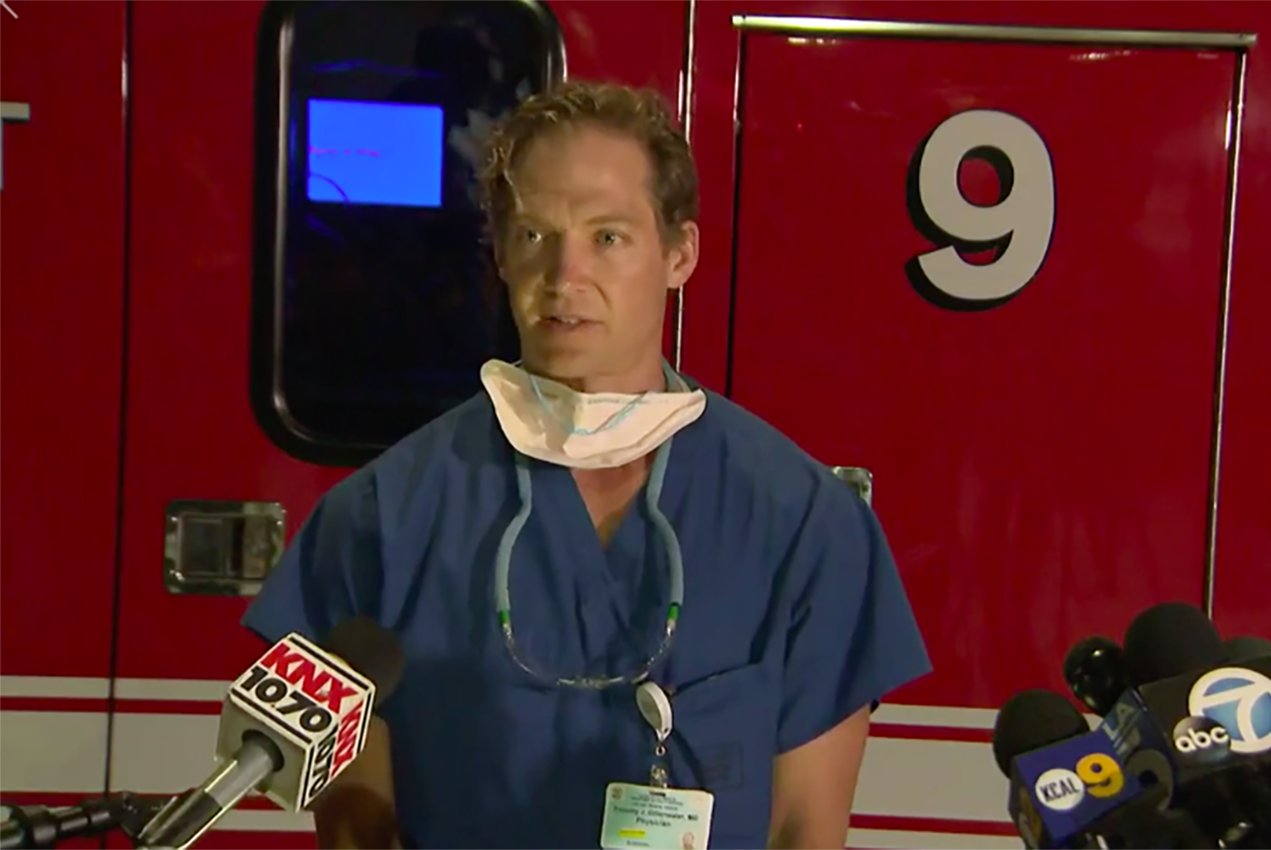
Justin Gillenwater, MD, MS, was walking in a park in Santa Monica with his wife and baby on Saturday, May 16, when one of his surgical residents who lives in Los Angeles’ Little Tokyo neighborhood started texting him photos: A building had caught fire, and the stored butane oil inside had exploded. Firefighters who were in the building essentially had to walk through a ball of fire to get out.
“I knew there would be mass casualties. I had to get in as quickly as possible.” Gillenwater, the medical director for the Southern California Regional Burn Center at Los Angeles County + USC Medical Center, raced across town. Eleven firefighters were raced to the Burn Center.
“I have been at the Burn Center since 2015,” said Gillenwater “We train and plan for disasters as part of our advanced burn life support, but I hadn’t seen anything like this before. A few of our nurses have been in the Burn Center for 30 years, and they hadn’t seen anything like this.”
Fortunately, the Burn Center is a part of LAC+USC’s Level 1 Trauma Center. “We’re the only Level-1 Trauma Center in the county that also has a burn unit,” Gillenwater explained. That was crucial, because the firefighters had access to the Emergency Department’s abilities to stabilize, triage and treat such a large number of people at the same time.
By the time Gillenwater arrived, the firefighters had their gear removed and were stabilized. Gillenwater met Alex Lacy, MD, the Burn Unit’s dedicated surgical fellow, plastic surgery chief resident Soleil Niknam-Bienia, MD, and in-house resident Casey Krebs, MD. They and the Emergency Department physicians gave him updates on all the patients. The firefighters had a range of injuries, ranging from first- to third-degree burns, and had been triaged according to the severity of their injuries.
“This would not have been possible with our Emergency Department,” said Gillenwater. “There’s a reason it’s one of the best-regarded programs in the country.”
Gillenwater worked with his colleagues to check the firefighters for hot gas and smoke inhalation injuries. Inhaling smoke, heated gases and particles from a fire can damage the lungs and throat and constrict breathing. A few of the firefighters were intubated and temporarily put on ventilators to make sure they could get enough oxygen into their systems.
Once all the firefighters had been extubated, it was time to treat their burn injuries.
Gillenwater first tended to a firefighter who had very deep burns and needed an escharotomy, a surgical removal of burned tissue in order to restore blood flow. “With a third-degree burn, the tissue becomes stiff and inflexible,” explained Gillenwater. “If there’s swelling, it can cut off the blood flow to healthy tissue.”
Gillenwater made careful evaluations for each patient. Though he is board-certified in both plastic surgery and critical care surgery, in many cases he says his most important decision is when not to perform a surgical procedure.
“Surgery causes scarring, and every scar has a consequence,” he explained. “I try to think about every patient’s mobility, comfort and even their appearance for 10, 20, or 30 years down the road. My philosophy is not to operate on wounds that will heal on their own with minimal scarring.”
Haig Yenikomshian, MD, chief of the Plastic Surgery Program at LAC+USC and one of the attending surgeons at the burn unit, pointed out that this is a unique advantage of the Southern California Regional Burn Center. “We’re the only burn unit in the country that is 100% run by a plastic surgery program. All of our attending surgeons — Dr. Gillenwater and I and Dr. Warren Garner — are dual-certified in plastic surgery and critical care surgery, and that’s crucial. When we treat acute burns, we think years or decades in advance. We want to make sure our patients can return to their lives.”
This long-term approach to care is exactly why Gillenwater chose to specialize in burn injuries and scarring. “I like the fact that I’m building a relationship with my patients. I get to take care of somebody from day one after a devastating event, through the healing process, and then I take care of their scars down the road. It’s rewarding to see patients come back from a trauma and get back to their lives.”
Gillenwater also likes the Burn Center’s team-based approach. Doctors, nurses, therapists, nutritionists, social workers, psychologists and pharmacists all work together to make sure that everyone gets the best possible care. “We talk about every patient as a group, and everyone has a voice in that patient’s care,” he said. “If any piece of that was missing, we wouldn’t have the good outcomes that we do. We use a team approach for every patient, every day.”
Gillenwater also made sure to point out that in addition to the incredible work from Emergency Department personnel, LAC+USC’s team was immediate and generous with resources. “I got a text from every hospital administrator that night saying, ‘What do you need and how can I help?’ The Chief of Surgery, the CMO, the CEO — everyone was on board immediately. That is collaboration.”
The most important thing is that every single firefighter injured in the blaze will survive. “That’s a testament to their gear and to the collaboration of everyone on the many teams who rushed in to help,” said Gillenwater. “Everyone pitched in, any way they knew how.”
— Lex Davis