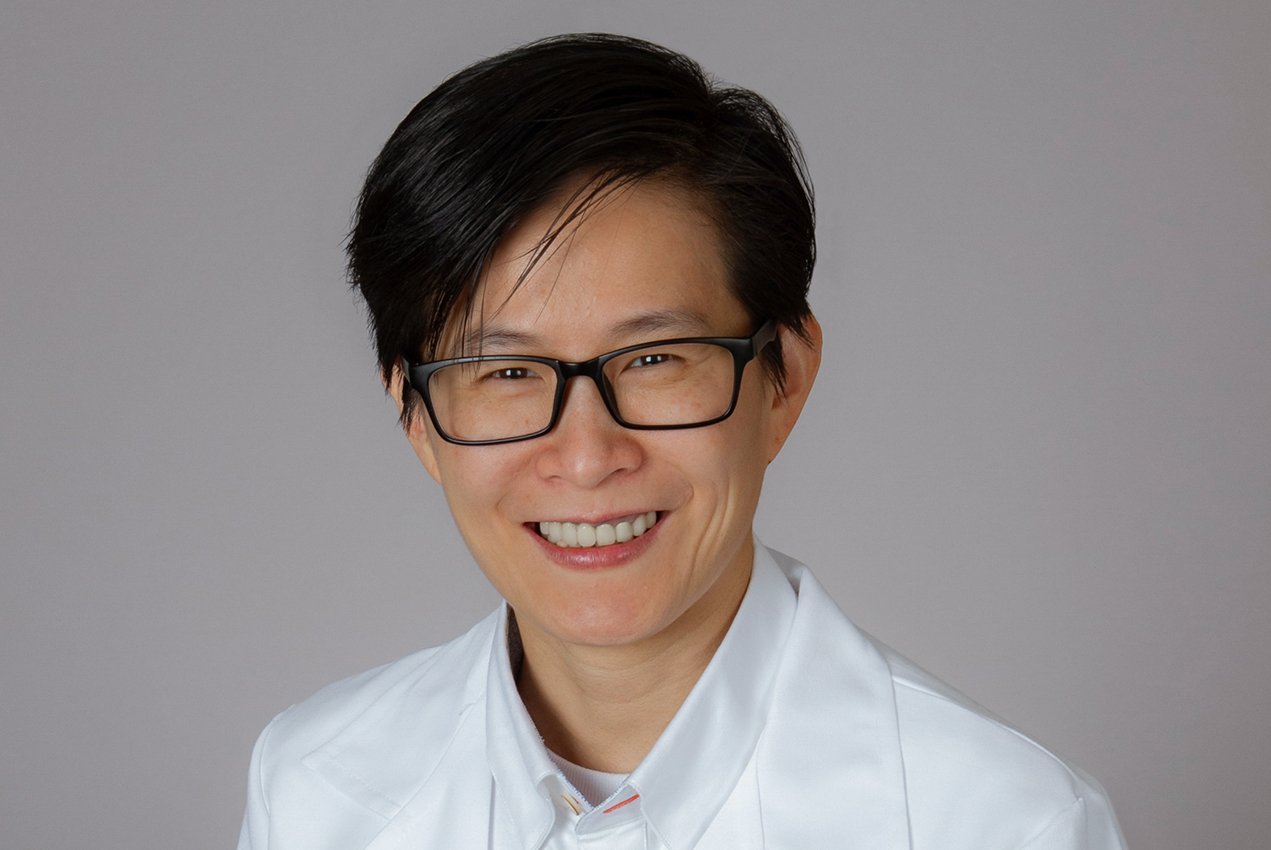
As the COVID-19 outbreak escalated into a pandemic, Keck School of Medicine of USC lung researcher Ya-Wen Chen, MD, PhD, expected to be spending a lot of time at home, sheltering in place.
“At the beginning of the quarantine, I was going to focus on writing grants,” said Chen, who joined the Keck School as an assistant professor of medicine plus stem cell biology and regenerative medicine in 2019. “I also wanted to spend time cleaning my house, cleaning my backyard, getting everything on track.”
Instead, Chen realized that her laboratory possesses a key resource to advance the fight against COVID-19: mini human lungs grown from stem cells. These lab-grown lung structures, known as organoids, provide a safe way for scientists to test potential anti-viral treatments that might fight the virus that causes COVID-19.
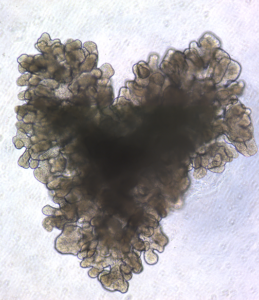
Chen’s lab uses human stem cells to study lung development, injury and disease. One of the lab’s major goals is to find a method for mass producing large numbers of identical lung organoids. These organoids could be used to screen thousands of potential drugs to treat pulmonary fibrosis, as well as several infectious diseases.
One of these diseases is COVID-19. The lab is working to develop an antiviral to prevent the virus that causes it from entering the cells that line the lungs, called the epithelium. Our lung epithelial cells contain a receptor called ACE2, along with an enzyme called TMPRSS2. The virus uses this enzyme as a key to “unlock” ACE2, which then becomes an entry point for invading and heavily infecting the lung cells. Chen’s team is using lung organoids to test whether an antibody can block the enzyme, locking out the virus.
To test another potential antiviral that might protect the lung cells involved in gas exchange from the virus, Chen is collaborating with Justin Ichida, PhD, who is the John Douglas French Alzheimer’s Foundation Associate Professor of Stem Cell Biology and Regenerative Medicine at USC. To support this research, the California Institute for Regenerative Medicine (CIRM) has awarded the team $150,000.
Other projects in the lab involve everything from growing blood vessels to support lung organoids, to regenerating the trachea and airway to help patients with genetic diseases such as congenital tracheal stenosis.
“For me,” said Chen, “I always want to fulfill my curiosity to find the answer.”
— Cristy Lytal