Accelerated healing isn’t just for superheroes. A new study in Cell Reports suggests a way that mere mortals can potentially speed their recovery from a wide variety of injuries.
“Our research shows that by priming the body before an injury, you can speed the process of tissue repair and recovery, similar to how a vaccine prepares the body to a fight infection,” said lead author Joseph T. Rodgers, PhD. He began the research during his postdoctoral studies at the Stanford University School of Medicine, and continued it in his current position as an assistant professor of stem cell biology and regenerative medicine at USC.
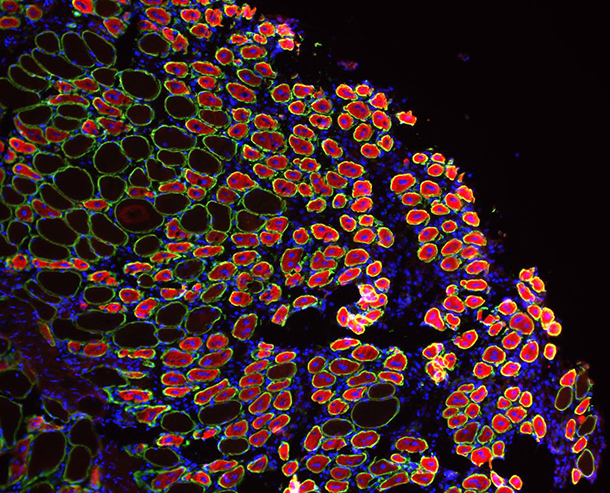
This recent study builds upon Rodgers’ previous finding: When one part of the body suffers an injury, adult stem cells in uninjured areas throughout the body enter a primed or “alert” state, giving them an enhanced potential to repair tissue damage.
In this new study, Rodgers and his colleagues identified the critical signal in blood that alerted stem cells: an enzyme called hepatocyte growth factor activator (HGFA), which is abundant in the blood but inactive until an injury occurs.
Rodgers and his colleagues then asked the question: What happens if HGFA alerts stem cells before an injury occurs? Does this improve the repair response? According to their research, mice that received HGFA prior to an injury healed faster, began running on their wheels sooner and even regrew their fur better than mice that did not receive the HGFA booster.
These findings indicate that HGFA can alert many different types of stem cells, rousing them from their normal resting or “quiescent” state, and preparing them to respond quickly and efficiently to injury.
“We believe this could be a therapeutic approach to improve recovery in situations where injuries can be anticipated,” said Rodgers, “such as surgery, combat or sports,” he continued, as well as for people with impaired healing abilities, such as older adults or diabetics.
“This work shows that there are factors in the blood that control our ability heal,” Rodgers said. “We are looking at how HGFA might explain declines in healing, and how we can use HGFA to restore normal healing.”
Co-authors include senior author Tom Rando, MD, PhD; Matthew Schroeder and Cynthia Ma. Funding came from the National Institutes of Health (grants AG041764, AG036695 and AR062185), the Department of Veterans Affairs, The Donald E. and Delia B. Baxter Foundation and the Glenn Foundation for Medical Research, and Stanford’s Department of Neurology and Neurological Science. —Cristy Lytal