Some people are better than others at recovering from a wounded heart, according to a new USC Stem Cell study published Aug. 7 in Nature Genetics.
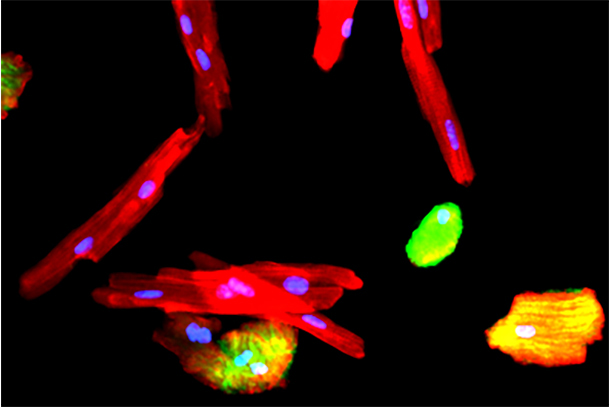
In the study, first author Michaela Patterson, PhD, a postdoctoral scholar – fellowship trainee at the Keck School of Medicine of USC who works in the laboratory of Henry Sucov, PhD, and her colleagues focused on a regenerative type of heart muscle cell called a mononuclear diploid cardiomyocyte (MNDCM). Zebrafish and newborn mammals, including mice and humans, have large numbers of MNDCMs and a relatively robust ability to regenerate heart muscle. Adult mammals have few MNDCMs and a limited capacity for regeneration after an injury such as a heart attack.
Even so, the situation for adult mammals is not uniformly dire: Patterson and her co-authors observed variation in the number of MNDCMs among different strains of adult mice. In some strains, MNDCMs accounted for only 1.9 percent of heart muscle cells. In others, a full 10 percent were MNDCMs. As expected, the higher the percentage of MNDCMs, the better the mice fared in regenerating heart muscle after injury.
The researchers then identified a key gene underlying this variation: Tnni3k. By blocking this gene in mice, the researchers produced higher percentages of MNDCMs and enhanced heart regeneration. In contrast, activating this gene in zebrafish decreased MNDCMs and impaired heart regeneration.
“The activity of Tnni3k can be modulated by small molecules, which could be developed into prescription drugs in the future,” said Sucov, senior author and professor of stem cell biology and regenerative medicine at the Keck School. “These small molecules could change the composition of the heart to contain more of these regenerative cells, as a preventive strategy for those at risk for heart failure.”
Ninety percent of this work was supported by $1.08 million of private and non-federal funding from three sources: a Doerr Stem Cell Challenge Grant; an award from USC’s Provost Office; and a California Institute for Regenerative Medicine Training Grant (TG2-01161). Ten percent was funded by $120,000 from National Institutes of Health grants (NHLBI NRSA 1F32HL124932, K08HL121191, HL123295, HL114137, and NS083265).
— Cristy Lytal