If anyone has a clear vision of the power of stem cell cures, it’s Anna Kuehl. She suffered a retina-wrecking disease that cost her much of her sight before USC physicians surgically implanted stem cells to restore her ability to see.
Today, she can see the letters on computer keys, use her iPhone and read billboards. She can see Catalina Island and ships and lights offshore from her Palos Verdes home in Southern California. Clarity gained has afforded her a brighter future based on stem cell therapies.
“It was like a miracle, the whole experience was so positive,” said Kuehl, 79, a Trojan alumna. “I’m the beneficiary of all the good people who were involved” with the USC Stem Cell initiative, she said.
After more than a decade of intensive research, stem cell solutions are happening, offering hope for millions of people in the form of gene therapies, better drugs and precision medicine. The cures may not be as fast as needed — building the scientific foundation for stem cell therapies takes time — but some research has already moved into human clinical trials.
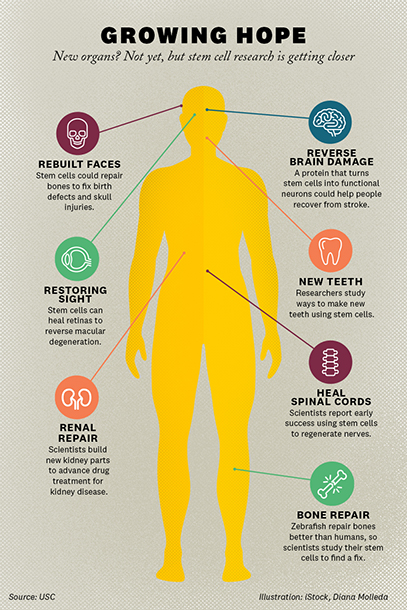
Yet, at USC and in labs across the United States and world, the clinical trials have shown promising preliminary results. For example, scientists have recovered sight for people, restored locomotion to paralyzed patients and freed babies imprisoned by disease. Current projects at USC range from understanding kidney development to engineering new bone to performing large drug screens on cells derived from patients with Lou Gehrig’s disease (ALS). The gains thrust USC and California into a leadership role in the field.
Progress will be on display next week when some 4,000 scientists converge on the International Society for Stem Cell Research (ISSCR) annual meeting at the Los Angeles Convention Center, two miles from USC. It’s the largest gathering of stem cell experts in the world. USC Stem Cell is the co-sponsor.
The ISSCR conference represents a triumph for science and society. It’s a reveal party for Los Angeles’ growing biomedical industry, an economic driver powered by USC and other universities and emergent biomedical companies in the region.
“People think of L.A. as an entertainment capital, but they don’t think of L.A. as having breadth and depth of science and research,” said Andrew McMahon, PhD, director of the Eli and Edythe Broad CIRM Center for Regenerative Medicine and Stem Cell Research at USC. “So this is a statement-making conference. It’s about USC and other universities, across L.A. and California, emerging as a biomedical center for world influence. It’s L.A.’s moment to shine as a city for science.”
How the USC Stem Cell initiative came to be
(Illustration/Diana Molleda)
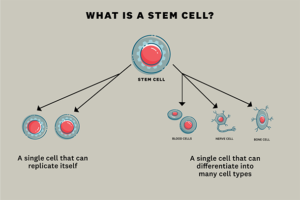
Stem cells are like seeds. They begin small and grow in complexity. Like seeds, they can grow into specialized parts; some turn into blood or nerve cells while others develop into muscle, bone or other tissues. Some grow just enough to repair damaged cells.
Stem cells can be derived from embryos or fashioned by reprogramming adult cells, under the right conditions, to assume a stem cell-like state called pluripotent stem cells, according to the National Institutes of Health (NIH).
Stem cells can become new tissue for use in transplants. They can show how disease progresses at a cellular level. They can be used to test new drugs.
The opportunity to build something from nothing attracted McMahon to USC from Harvard University in 2012. He came to USC to launch the USC Stem Cell initiative. It was a once-in-a-lifetime opportunity to grow something new, leveraging the intellectual capital within the university’s 23 schools. It was a chance to grow a biomedical industry in L.A. And grow it did.
Today, the USC Stem Cell initiative involves 104 research labs across the University Park and Health Science campuses and Children’s Hospital of Los Angeles. Twenty-two of these labs comprise the Broad Center, which serves as the hub of a larger initiative supported by about 100 researchers across the university.
At USC, stem cell research is a three-pronged effort: the stem cell department at the Keck School of Medicine of USC; the Broad Center; and a university-wide initiative to connect all stem cells scientists and clinicians.
Funding comes from the NIH, which provided USC stem cell researchers with $81 million in research grants this year. The California Institute for Regenerative Medicine (CIRM) has provided $136 million over the past seven years. And private fundraising totals about $75 million, including contributions by The Eli and Edythe Broad Foundation.
“This is an example of one of the major areas of research that extends across USC,” said Randolph Hall, vice president of research for USC. “It involves engineers, artists, dentists, computer scientists, ophthalmologists, physicians and more. California instituted a unique public funding program through which USC could conduct innovative and interdisciplinary stem cell research that matters to patients.”
Cross-discipline treatments can mean cutting-edge successes
The ambition of the USC Stem Cell enterprise is evident as convergence across academic disciplines has advanced innovative approaches to curing diseases.
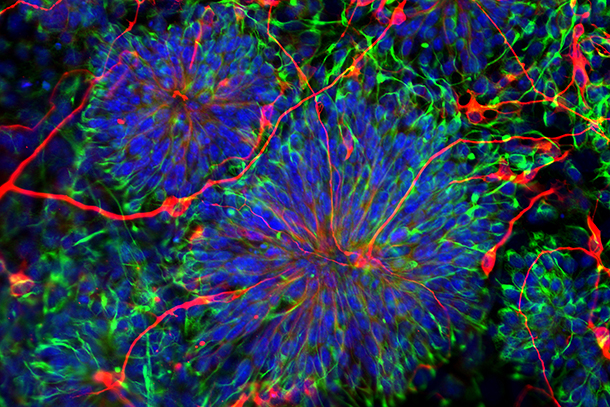
For example, researchers report progress against age-related blindness, a disease that robs the vision of 30 million to 50 million people worldwide, mostly senior citizens. Also known as macular degeneration, it’s the focus of a USC Stem Cell Public Symposium on June 26 at the Health Sciences Campus.

After her vision deteriorated due to dry macular degeneration, Anna Keuhl received a stem cell-based retinal transplant. (Photo/Tracy Boulian and David Ahntholz)
Kuehl suffered from a dry macular degeneration, the most common form and exceedingly difficult to treat. It began robbing central vision in her left eye about 30 years ago. The condition creates a black area in the center of a person’s field of vision as the macula — a part of the retina behind the eye — breaks down. She could no longer drive a car or discern faces or the time on her watch. She was going blind.
“All of a sudden, I saw this big, black area [of vision] and I was so surprised and scared that I called the USC [Gayle and Edward Roski] Eye Institute right away,” Kuehl said.
Enter USC’s Mark Humayun, MD, PhD, who — with a team of surgeons, engineers and scientists — used stem cells to treat Kuehl. Humayun is co-director of the USC Roski Eye Institute and a University Professor of Ophthalmology. The team’s surgeon, Amir Kashani, MD, PhD, assistant professor of clinical ophthalmology at the Keck School, installed a tiny, stem cell-laden patch inside Kuehl’s eye, which began to repair the damage. It’s one technique that shows promise among six clinical trials underway worldwide to treat macular degeneration.
“With the right kind of environment and support, you can actually treat very specific regions or diseases down to the cellular level,” Humayun said. “One aspect of that could be called precision medicine, and another aspect is that stem cell-based therapies are coming of age. This will be one of the first studies to land that point.”
USC Stem Cell: a university-wide effort
The USC Stem Cell initiative is nurtured by a culture of collaboration and innovation. Experts across many of the university’s 23 colleges are involved.
There have been contributions from computer scientists at the USC Viterbi School of Engineering; pediatricians at Children’s Hospital Los Angeles; dentists at the Herman Ostrow School of Dentistry of USC; biologists at the USC Dornsife College of Letters, Arts and Sciences; geneticists at the USC Leonard Davis School of Gerontology; and surgeons at the Keck School of Medicine of USC. The new USC Michelson Center for Convergent Bioscience also functions as a syncretic catalyst to advance health science research across the university.
Researchers focus on stem cell applications for some of the worst maladies, including cancer, ALS, heart disease, arthritis, diabetes, kidney disease and birth defects, among others.
The USC Stem Cell program is young. At just 7 years old, it’s a new program exploring new paths, and it’s attractive to younger scientists seeking entrepreneurial energy. The USC program is being built for the long game, McMahon said, to find stem cell solutions for human diseases for years to come.
“I decided to join this department because it has a culture that drives innovation,” said Giorgia Quadrato, PhD, a new assistant professor of stem cell biology and regenerative medicine at the Keck School. “This is due to the fact that there are so many junior faculty. And so there is this culture of embracing creativity, because junior faculty are fresh and are not bound by dogma.
“I really like also that this innovative and collaborative culture extends to the broader USC community, which supports and encourages multidisciplinary collaborations.”
California’s role in advancing stem cell research
(Illustration/Diana Molleda)
California has proven fertile soil for stem cell research. The state has assumed a leadership role in stem cell science since voters approved Proposition 71 in 2004, which seeded the industry with $3 billion in bond funds. The program is administered by CIRM, which contributes about 30% of USC Stem Cell funding.
The Broad Center at USC was funded through a $30 million gift from The Eli and Edythe Broad Foundation, a $27 million grant from CIRM and monies donated through private philanthropy. The center is located on USC’s Health Sciences Campus in Boyle Heights.
Other California universities — including UCLA and the University of California, San Francisco — and companies within the stem cell ecosystem help drive the growing life science industry in California.
“You shine through the reflection of other people you work with,” McMahon said. “We get great research collaborations and convergence across the institutions. We work across universities and research institutions to build teams, add expertise and attract resources, facilities and people. It all accelerates the pace of research and it’s all driven by the energy and vitality of the Los Angeles area.”
Synergy is evident in economic analyses developed by trade groups like the California Life Sciences Association (CLSA) and San Diego-based Biocom Life Science Association of California. Their data shows the life science industry, of which stem cell science is a significant contributor, is one of the fastest-growing segments of the California economy.
For example, the life sciences industry in California accounted for $178 billion in revenue and at least 311,000 jobs in 2017. California companies have at least 1,300 potential therapies in the pipeline to help people facing cancer, infectious diseases and rare and genetic diseases, among other conditions, according to the CLSA.
In Los Angeles County, life science-related jobs accounted for 11% growth in jobs in research and laboratory services. The county received nearly $1.1 billion in funding from the National Institutes of Health, tops for any county in California, according to Bicom’s 2018 economic impact report.
“The life science industry remains a highly important economic engine for Los Angeles County,” the report said.
The upcoming ISSCR conference marks the first time that the event — the largest gathering of its kind in the world — has come to L.A. By the numbers, more than 4,000 people are expected to attend, 200 speakers to present, 100 companies to promote and 35 scientific sessions to occur during the conference.
“L.A. is the latest and most innovative bioscience hotspot in the state, and ISSCR’s choice is a reflection of the scientific advances occurring in our city today,” said L.A. Mayor Eric Garcetti.
Research meets a financial and electoral crossroads
With progress comes growing pains, and California’s stem cell program is at a crossroads.
On one hand, gains in the lab have moved stem cell therapies closer to making a significant impact on medicine. Yet, the complexity and cost of cellular medicine has proven a big challenge. Scientists acknowledge it will be difficult to cure major diseases with stem cells. The gap between hype and hope has narrowed, but not closed.
“Hype can be right, but it’s the time frame when people expect things to happen that can be wrong,” McMahon said. “Curing cancer, diabetes, Alzheimer’s and other diseases is taking longer and involves a lot more complication and funding. The progress has been astounding — but it’s never fast enough.”
State funding for stem cell research under CIRM is expected to run out this year. The $3 billion ballot initiative that voters approved — Proposition 71, the California Stem Cell Research and Cures Act — is substantially depleted. Other sources, such as federal funding, private investment and philanthropy, are available but not necessarily dedicated to statewide research. CIRM funds have played a big role in creating and sustaining the USC Stem Cell initiative.
Researchers are hopeful California voters will have an appetite to continue funding. Backers of Proposition 71 are planning a $5 billion measure for the November 2020 ballot. With research gains and clinical trials underway, backers are hopeful California will continue to support progress for another decade.
Eli and Edythe Broad CIRM Center for Regenerative Medicine and Stem Cell Research (Photo/Steve Cohn)
Yet, voter perception of stem cells could be colored by rogue clinics peddling dubious wonder cures like snake oil. Those businesses operate outside the realm of leading research institutions such as USC. More than 100 such stem cell clinics operate in California alone. The Food and Drug Administration is stepping up enforcement actions against clinics offering unapproved stem cell products that endanger the public.
At the same time, the momentum toward stem cell therapies at USC and other universities is undeniable. On the trail to finding breakthroughs for big diseases, basic research has unlocked a host of co-benefits — many unforeseen when California embarked on its stem cell program 15 years ago — that are valuable to medicine.
For example, stem cell research has increased basic understanding of how diseases occur. By watching stem cells mature into cells into tissue and components of organs, doctors and scientists better understand how diseases develop.
Stem cells can also be used to generate healthy new cells to replace diseased cells, known as regenerative medicine. Stem cells can be guided into becoming specific cells that can be used to regenerate and repair diseased or damaged tissues in people.
And stem cells are proving useful for testing new drugs for safety and effectiveness. By growing tissue in a lab — which is now doable with heart and kidney tissue — scientists can experiment with drugs more easily and report findings more quickly, which are important steps to hastening the drug-discovery process. In general, it takes millions of dollars and years to bring new drugs to market.
Stem cell successes seem like near-miracles
Some aspects of stem cell science seemingly border on the miraculous.
For example, researchers used an approved stem cell treatment to help a young man paralyzed in a car accident. Kris Boesen of Bakersfield was injured when his car crashed into a tree in 2016. A surgical team from Keck Medicine of USC and Rancho Los Amigos National Rehabilitation Center injected him with an experimental treatment made from stem cells as part of a multi-center clinical trial. The treatment helped him regain use of his arms and hands.
Researchers at St. Jude Children’s Research Hospital and UC San Francisco used stem cells and gene therapy to cure eight babies with severe combined immunodeficiency, the so-called “bubble boy disease.”
And clinical trials to treat macular degeneration — the disease that afflicts Trojan alumna Kuehl — are beginning. Research teams at USC, the NIH and a San Diego biomedical company are pursuing various methods using stem cells to treat the disease.
Once an avid hiker, Kuehl is on the trails again. She remembers when impaired vision necessitated going to the print shop to make huge enlargements of trail maps. She remembers when she had to carry a magnifying glass to read trail markers. She remembers when she had to curtail her love of hiking because it was difficult to navigate uneven terrain. Since her treatment, she can see the path ahead. She’s confident her story will help others see the value of approved stem cell therapies.
“I’m interested in science, and I try to help further science whenever I can. Science is good when used in ways like this to benefit people,” she said.
— Gary Polakovic