Even though the transplantation of blood stem cells, also known as bone marrow, has saved lives over many decades, the genes that control the number or function of blood stem cells are not fully understood. In a study published in June in Stem Cell Reports, the USC Stem Cell labs of Hooman Allayee and Gregor Adams uncovered new genes that affect blood stem cell development and maintenance.
The Allayee and Adams labs performed a genetic screen of a collection of more than 100 mouse strains that are commonly used in laboratories, called the hybrid mouse diversity panel.
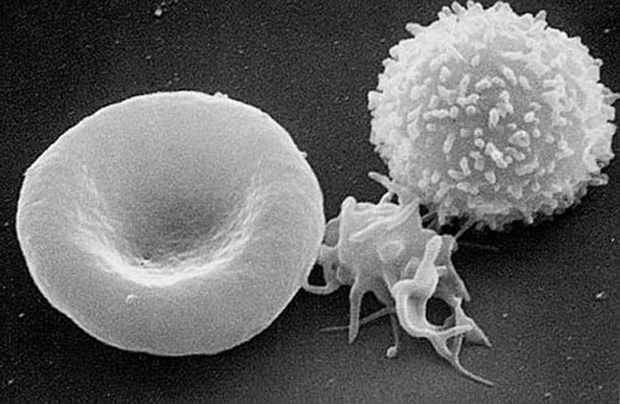
The researchers found that different strains have different numbers of several important sub-populations of blood stem cells, including so-called short-term HSCs, which are responsible for the formation of red and white blood cells in adults. The activation of a gene called Hopx is associated with an increased number of short-term HSCs. The researchers further proved this finding by showing that mice lacking the Hopx gene form fewer short-term HSCs and are ineffective bone marrow donors.
“Short-term HSCs are the major stem cells in the adult bone marrow, so finding new genetic regulators of this subpopulation may have clinical benefits,” said Adams, PhD, an assistant professor of cell and neurobiology at the Zilkha Neurogenetic Institute and the Keck School of Medicine of USC.
More broadly, the researchers have shown that the hybrid mouse diversity panel can be used to find genes that would otherwise go unnoticed.
“This powerful genetics platform has the potential to reveal the genes underlying other stem cell populations or a wide range of diseases that would be difficult to study in humans,” said Allayee, PhD, an associate professor of medicine at the Keck School.
The paper’s lead authors are Xiaoying Zhou and Amanda L. Crow from USC. Additional contributors include Jaana Hartiala, Tassja J. Spindler and Lora W. Barksy from USC and researchers from UCLA, the University of North Carolina, Chapel Hill and the University of Pennsylvania.
This work was supported by grants from the California Institute for Regenerative Medicine, the National Institutes of Health and the Margaret E. Early Medical Research Trust.
— Marie Rippen