By Cristy Lytal
Three newly assembled research teams within USC Stem Cell, the regenerative medicine initiative at USC, will take steps that could lead to future stem-cell based therapies for certain forms of deafness, bone defects and pediatric leukemia.
The teams are the winners of USC’s Regenerative Medicine Initiative (RMI), a University-wide program kick-started by $1.2 million in funding from the office of Carmen A. Puliafito, MD, MBA, dean of the Keck School of Medicine of USC. Each RMI Award provides up to $200,000 per year for two years to multi-investigator research collaborations that harness the full potential of USC-affiliated faculty members.
“We hope these are the first of many awards as we continue to develop new strategies to enable and empower regenerative medicine researchers across USC,” explained Andrew McMahon, PhD, director of the Eli and Edythe Broad Center for Regenerative Medicine and Stem Cell Research at USC, who is spearheading USC Stem Cell and the RMI Awards.
The three winning teams were selected from 26 proposals, involving 80 faculty members from Children’s Hospital Los Angeles (CHLA); the USC Viterbi School of Engineering; the USC Dornsife College of Letters, Arts and Sciences; the House Ear Institute; the USC School of Pharmacy; the Ostrow School of Dentistry of USC; and the Keck School of Medicine.
For the first team, Neil Segil, PhD, and Takahiro Ohyama, PhD — both from the House Ear Institute — will work with Justin Ichida, PhD, assistant professor of stem cell biology and regenerative medicine, on curing deafness by using cellular reprograming to create inner ear cells, including sensory hair cells. The death of these cells, which humans and other mammals cannot regenerate, is the most common cause of deafness.
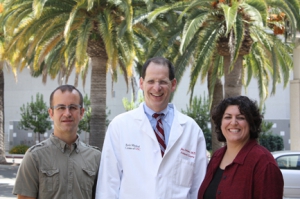
Gage Crump, Jay R. Lieberman and Francesca Mariani comprise one of the winning RMI teams who will be performing multi-investigator collaborations as part of USC’s regenerative medicine initiative. By studying mice and zebrafish, their team will focus on ways to repair human bones through the use of osteoblasts. (Photo/Cristy Lytal)
The second team will focus on ways to repair human bones through lessons learned from mice and zebrafish. When mouse ribs or zebrafish jaws are damaged, special cartilage cells transform into bone-producing cells called osteoblasts. The team hopes to show that osteoblasts can effectively heal severe bone damage.
The project brings together Jay R. Lieberman, MD, a clinical orthopaedic surgeon and chair of the Department of Orthopaedic Surgery; and assistant professors of cell and neurobiology Gage Crump, PhD, and Francesca Mariani, PhD.
The third team will develop therapy for B-precursor acute lymphoblastic leukemia (BPL), the most common form of cancer in children and adolescents. Some children with BPL have a genetic defect that results in the production of an abnormal form of the protein CD22E12, which causes their cancer stem cells to proliferate and resist chemotherapy. The team will use insights gained from studying CD22E12 to design new and more effective treatment strategies.
Fatih Uckun, MD, PhD, professor of research pediatrics who heads the translational research in leukemia lymphoma at the Children’s Center for Cancer and Blood Diseases of CHLA, and Gregor Adams, PhD, assistant professor of cell and neurobiology, are co-principal investigators on the project. They will collaborate with Frank Alber, associate professor of biological sciences at USC Dornsife, and colleagues across multiple campuses.
“I view this as an opportunity to work together with my colleagues,” said Uckun. “Only by working as a team can we accomplish the goal of helping children who are in urgent need of a new treatment.”

