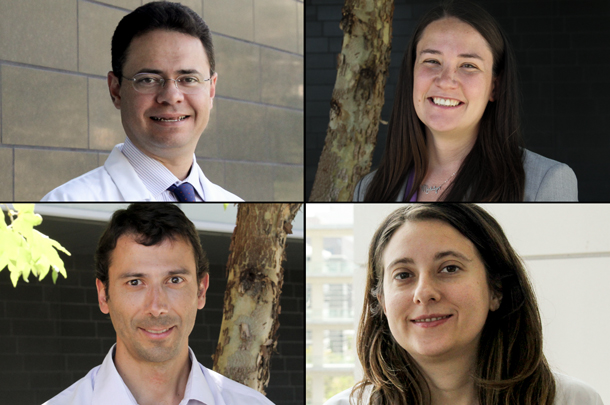
This year, the Broad Clinical Research Fellowships are enabling physician investigators to explore stem cell-based approaches related to four very different medical conditions: breast cancer, kidney disease, deafness and short bowel syndrome.
Each one-year fellowship provides $65,000 of salary support, $7,500 of supplies and a $1,500 meeting allowance to support full-time research related to stem cell biology and regenerative medicine. The fellowships are potentially renewable for a second year.
A clinician who received his urology training in Brazil with an additional clinical fellowship in robotic urologic surgery at USC, Andre Luis de Castro Abreu, MD, will focus on kidney regeneration.
He will take a close look at a newly discovered mechanism of kidney repair regulated by the organ’s population of macula densa (MD) cells, which sense and communicate subtle changes in salt concentration, fluid flow and other metabolic factors.
The USC laboratory of Janos Peti-Peterdi, MD, PhD, has developed a new imaging technique to observe this repair mechanism in living mouse kidneys. Abreu will use this imaging technique to confirm that this repair mechanism is also present in human kidneys, and to learn more about it.
“These studies are expected to result in potentially groundbreaking new discoveries, which may lead to the future development of new therapeutic approaches for the better treatment of cardiovascular and kidney diseases,” said Abreu, who will be co-mentored by Inderbir Gill, MD, professor and chair of the USC Department of Urology, and Peti-Peterdi, professor of physiology and biophysics. “It is an honor to be a Broad Clinical Research Fellow and to work with this team.”
A third-year medical oncology fellow, Victoria Forte, MD, will determine whether cancer stem cells (CSCs) are present in the blood of non-metastatic breast cancer patients, both pre-treatment and at least one-year post-treatment. By detecting and analyzing these cells using highly sensitive tools and techniques, Forte hopes to determine whether the cancer can be targeted and eradicated post-treatment of newly diagnosed breast cancer, thus preventing eventual recurrence.
Forte will also enroll in two courses offered through USC’s Master’s of Stem Cell Biology and Regenerative Medicine, plus an eight-week training course sponsored by the Southern California Clinical Translational Science Institute on clinical and translational research study design.
“This research fellowship will prepare me with the necessary training to become a breast cancer translational researcher who will focus on how to target and eradicate circulating cancer stem cells,” said Forte, who will perform this project in the laboratory of Julie Lang, MD, FACS, at the USC Norris Comprehensive Cancer Center with additional mentorship from Min Yu, MD, PhD, in the Eli and Edythe Broad Center for Regenerative Medicine and Stem Cell Research at USC.
A practicing neuro-otologist who received his medical training in Spain, Rodrigo Martínez Monedero, MD, PhD, will work to understand why deafness is permanent in humans and other mammals. In species such as birds, the inner ear’s supporting cells can “heal deafness” by changing into and replenishing the damaged sensory cells responsible for hearing. Martínez Monedero hypothesizes that mammals cannot replenish sensory cells because key genes in the supporting cells are either “turned on or off” through a process called epigenetic regulation. He hopes it will be possible to target specific epigenetic “on-off switches” to regenerate the inner ear and treat deafness.
“This fellowship will allow me to continue my interest in stem cells and the problem of hair cells and neuronal regeneration, and it will help in pursuing my goal of becoming an independent physician-scientist,” said Martínez Monedero, who will pursue the project in the laboratory of Neil Segil, PhD, at the Eli and Edythe Broad Center for Regenerative Medicine and Stem Cell Research at USC.
A surgeon in training, Kathy Schall, MD, will work to help children and adults with short bowel syndrome (SBS) avoid surgery. SBS occurs when a patient can no longer absorb adequate nutrition after a bowel resection, which is the surgical removal of intestines, as a result of the shortened length. The surgical treatments for SBS — which are either intestinal elongation operations or small intestinal transplantation — can result in serious complications or even death. To decrease the need for these risky surgeries, Schall is exploring ways to encourage the stem and progenitor cells to regenerate and increase the surface area of the remaining intestines.
Schall will investigate the molecular signals — including the Wnt signaling pathway — that trigger intestinal regeneration in zebrafish. She will also locate and identify stem and progenitor cells within the intestines.
“Future therapies improving stem and progenitor cell adaptation could prevent the need for highly morbid medical and surgical interventions,” said Schall, who will conduct her research in the laboratory of Tracy C. Grikscheit, MD, at Children’s Hospital Los Angeles. “I am humbled and honored to be selected as one of the Broad Clinical Research Fellows.”
In addition to providing these opportunities at USC, the Eli and Edythe Broad Foundation is supporting clinical fellows at UCLA and UC San Francisco. The three universities’ stem cell research centers were all established with support from Eli and Edythe Broad and the California Institute for Regenerative Medicine (CIRM).
As Andy McMahon, PhD, FRS, director of USC’s stem cell research center, said, “We are grateful to the Broads for their commitment to training of physician investigators because of their highly important role in the translation of stem cell biology toward patient care.”
— Cristy Lytal