By Jon Nalick
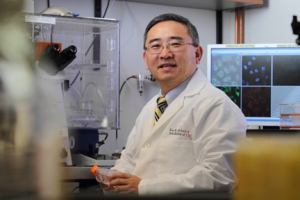
Principal investigator Jae Jung received a $7.5 million grant to help discover how to short circuit development of Kaposi’s sarcoma.
(Photo/Phil Channing)
The National Institutes of Health (NIH) have awarded Keck School of Medicine of USC researchers a five-year, $7.5 million grant to investigate how Kaposi’s sarcoma-associated herpesvirus (KSHV) evades the immune system and triggers certain cancers.
Principal investigator Jae Jung, PhD, the Fletcher Jones Foundation Chair and Hastings Foundation Professor of Molecular Microbiology and Immunology at the Keck School, said the research aims to find ways to short circuit the development of Kaposi’s sarcoma. This malignant tumor, often caused by KSHV, is more prevalent among people with compromised immune systems, such as patients with AIDS.
In Africa, he said, where AIDS is endemic and advanced medical treatment is spotty, Kaposi’s sarcoma causes as many as half of all cancer deaths.
The NIH grant, awarded through the National Institute of Cancer, will fund three related projects, led by Jung, Pinghui Feng, PhD, associate professor of molecular microbiology and immunology, and Shou-Jiang Gao, PhD, professor of molecular microbiology and immunology. Each project will be assisted by a genetic core, led by Paula Cannon, PhD, associate professor of molecular microbiology and immunology, and a virology core, led by Hyera Lee, PhD, research assistant professor of molecular microbiology and immunology.
The projects as a whole will examine various biochemical and immunological aspects of how KSHV eludes and manipulates the human immune system to persist indefinitely within the body — and how it initiates the growth of Kaposi’s sarcoma.
At present, Jung said, KSHV and other herpesviruses are especially difficult to attack medically: “Herpes is forever. We cannot get rid of it, and it stays with us until we die because the virus has a number of ways to establish a persistent infection. We hope our research will become the cornerstone of vaccine development and anti-viral therapy.”

